I knew I was doomed the moment I turned 25. Psychologists say that’s the age when your brain is finally done developing, so any hopes of my genetically tragic neurochemistry changing evaporated right when I blew out those birthday candles. Dammit.
I started showing severe anxious tendencies before first grade, and it turned depressive soon after. While my classmates were making cootie catchers, I was contemplating the purpose of life. You could say I’ve always been ahead of the curve when it comes to mental illness (humble brag). When my friends started navigating heavy emotions around puberty, I was miles ahead. I’d been there, done that, and had racked up the therapy bills to prove it. Honestly, the more self-work I’ve done over the years, the more I’ve grown afraid that mental illness is just hard-wired into me.
I heard about Mindbloom, an at-home ketamine therapy program, via the ads in one of my favorite murder podcasts. As a regular cannabis user, who’s admittedly no stranger to recreational drugs, I was intrigued. I suspected my 15-plus-year journey with talk therapy was plateauing, so I thought, why the hell not? If nothing else, it’ll make a good story. *Looks to camera.* My hope was that maybe the ketamine could help me shake the metaphorical rust off my mind and snap it out of those old, damaging patterns.
Cut to a few months later, I’m sitting in my childhood best friend’s apartment, trying to remember the instructions. Sit upright, now tilt forward, chin up—no, chin down. Chin down?
I put the powdery pressed tablet between my gums and cheek with an open mind. I was required to stay like this without spitting or swallowing for seven minutes as it dissolves. The taste is foul. When I hear the chime in Mindbloom’s app signaling time is up, my mouth is filled with saliva. I spit the medicine into a cup to safely dispose of later, fluff my pillow, toss a blanket over me, pull down my eye mask, and lay down, waiting for the drug to kick in.
And—spoiler alert—nothing happened.
It felt like a less-than-successful attempt at meditation. But I would soon learn I was wrong to assume the trip needed to be gnarly in order to have impact. That’s not really how ketamine therapy works. The dissociative psychedelic has been found, recently, to be effective against treatment-resistant depression, PTSD, and anxiety—check, check, and check; I’m three-for-three on those. You can find it in the form of IV therapy in some doctor’s offices and clinics. Hospitals are even prescribing ketamine nasal sprays for depressed patients.
The drug stimulates the regrowth of synapses that often break due to depression and puts the brain into a neuroplastic state. When you’re young, the brain is very impressionable—which is how you can learn so much in the first few years of your life—but it doesn’t stay that way. The older you get, the harder it is to make lasting marks on it. In fact, psychedelics are one of the few preferred avenues to do so. Psychiatrist Dr. René Stokes describes neuroplasticity as “our brain’s ability to shift and prune old circuitry and build new circuitry.” For three to five days after each ketamine session, your brain is more open to suggestion. It’s a good time to practice any changes you want to implement and new habits you hope to form, or break old habits altogether. Stokes, an expert on trauma’s cellular impact, calls the potential for ketamine therapy “profound,” noting that some patients report relief from symptoms they’ve been experiencing for up to 30 years. Plus, ketamine is one of the best tools for dramatically reducing suicidal thoughts, she says. The medicine’s remarkable effectiveness and results, she concludes, can’t be denied.
There are other companies like Better U and Field Trip, but Mindbloom is the country’s largest provider of psychedelic medicine and was recently included in the largest peer-reviewed scientific study on medicinal ketamine. The results proved the treatment to be effective across a broadly diverse patient demographic. Dr. Leonard Vando, the company’s medical director, says that 89 percent of clients felt improved symptoms, with 63 percent reporting the symptoms were cut in half or even greater. I certainly count myself in with the 89 percenters, but I’m not sure I feel so strongly as to say my symptoms have been halved.
The first steps in signing up for the program simply vet for eligibility. I answered questions like: Are you over 18? Do you have a depression or anxiety diagnosis? Do you reside in one of the 36 states where Mindbloom is active? (They legally can’t operate in certain states that mandate in-person visits prior to prescribing controlled substances.) If you pass that test, you get on a call with one of the clinicians, a.k.a. psychiatrists, psychiatric nurse practitioners, or physician assistants hired by Mindbloom to perform psychiatric evaluations on applicants and oversee treatments. In this preliminary meeting, I was asked about pre-existing health conditions, my mental health history, and symptoms, as well as my home life to make sure I had a calm, private space to conduct my sessions.
Next, I selected a “guide.” This part is kind of like picking a therapist. There are lots of guides to choose from, each with their own specialties. They come with backgrounds in practices like life coaching, addiction recovery, trauma healing, suicide prevention, or somatic techniques and receive additional training from Mindbloom. I opted for a young woman who struck me as middle-of-the-road. I was looking for that Goldilocks-level metaphysical belief similar to my own. Sometime before my initiation, my “Bloombox” came in the mail: a briefcase with space to store “the medicine,” a journal and pen, an eye mask, and a blood pressure cuff. The medicine for your first session comes securely in a separate package, along with anti-nausea medicine. My first dose was a standard 350 milligrams as prescribed by my clinician. This dosage, she later explained, mostly aims to establish that the client tolerates the medicine well enough to move forward.
The first session’s run of show goes like this: a 30-minute call with my guide to discuss what to expect, go over the instructions, and take my heart rate and blood pressure. Clients have to designate a “peer treatment monitor,” a trusted individual whose job is to visually check on the patient every 15 to 20 minutes during the 60-ish minute “trip.” Think of it like a drug babysitter. During this pre-treatment call, my monitor had to show her face on the video chat to prove that I wasn’t faking the supervision. (This is the only time I had to prove anyone was there with me. I wasn’t asked about my monitor again.)
We hung up, and alone in a quiet room, as you know, I felt nothing. When we got back on the phone to debrief—as is customary for the first session—she explained that perhaps the introductory dose was simply not strong enough for me, but finding that out is exactly what the first session is for. Only the first session follows this regimen of speaking with your guide immediately before and after.
For my second and third forays, my clinician increased the dose to 600 mg since 350 mg didn’t move the needle for me. It didn’t feel much different than the first, so we went up to 900 mg for my final three sessions. (This is one of Mindbloom’s higher dosages. For reference, in party settings, an average “bump” usually lands between 30 and 60 mg. K-holes come in at around 100 mg.) I had an “integration session” with my guide after the second session to unpack anything that might have arisen during the first sessions, which was approximately nothing for me, and then a wrap-up call after the last one.
Mindbloom recommends completing the program in six to eight weeks, scheduling sessions seven to 10 days apart. Naturally, life got busy, and I regrettably didn’t stick to such a concise schedule. Instead, I did my treatment over the course of three months. This flexibility and freedom is really nice, and a luxury you certainly don’t have with IV treatments.
While in-person IV treatments tend to go for $500–$1,000 per session, the cost for Mindbloom’s basic package—six sessions with all the materials, clinician check-ins, coaching and integration sessions—is $1,158. It boils down to just over $100 per session. It begs the question: Would you pay $1K to have a breakthrough in the comfort of your own home?
If I’m being honest, the first four sessions were underwhelming. All it did was put me in a mild meditative state. But as we increased my dosage, the sessions did get more impactful, transportive, and emotional. Still, it wasn’t anything too intimidating, at least for me. A bit trancelike, but I didn’t see talking horses or hear God’s voice or anything like that. There were faint, amorphous visuals, but my eyes were closed, after all. This is the best way I can describe it: If you’ve ever had a massage and felt like you “went somewhere,” that’s what it was like for me.
While the actual experience of the medicine was mild, I believe access to neuroplasticity is invaluable. I saw it as my chance to retrain and rewire my brain—to break it out of those patterns it was stuck in. “Especially for patients with trauma histories or pretty severe anxiety, that dissociative window allows them to do the work of reframing maladaptive or unhelpful thinking infrastructures which, when entrenched, that way of thinking continues to fuel their symptoms,” Stokes confirms. So, in the days after each session, I tried to be kinder and gentler with myself and to avoid those negative pathways that were so ingrained in me from a young age. It’s a trivial example, but I decided I would floss every night after each session, wishing that it would imprint on my brain, and I’d never need a filling ever again. Cavities, be gone!
I never had a breakthrough while under the influence, but I did have one during the midpoint integration session. I’ve always had a top-down approach to my problems, tackling things from a cognitive angle, but my guide had an interesting suggestion. Maybe, she said, I need to focus on my body. I can’t talk my way into feeling safe, she said. I have to feel my way into that.
It might seem like a basic revelation, but in all my years of therapy, this concept had somehow never come up. I knew that trauma is stored in the body, but I didn’t think that applied to me. I thought that type of trauma was reserved for survivors of physical abuse or violence. According to my guide, the same goes for those of us dealing with low-grade trauma. I never considered that I can’t simply think my way out of moods, and that’s why it never works. I can think all I want, but if my nervous system still feels frozen in survival mode, I will continue feeling that way. For the first time in nearly two decades, I have a new approach, one that makes me hopeful that there’s real progress to be made, that I can feel better.
Now that all is said and done, do I think ketamine therapy worked? I wasn’t sure at first. This year was really hard. It knocked the wind out of me. Life does a good job at keeping you distracted, and it’s hard to clock growth or progress when you’re constantly spinning your wheels through whatever inevitably comes up. Like Lucille Ball in the chocolate factory sketch, except the chocolates are the hurts and frustrations—big and small—that just come with existing. I didn’t have a stable baseline from which to evaluate the ketamine’s efficacy as I had hoped. But the more I think about it, the more I believe the treatment helped me to tread water in a tumultuous season of life. It helped me avoid spinning deeper into depression. No, it wasn’t what I thought it would be—is anything ever?—but I’m counting it as a net positive. Can I definitively say this difficult year would have been even worse without Mindbloom? There’s no way to know, but I do feel better off. Plus, I am flossing more, albeit not nightly.
The medicine was a reminder that I can feel good. Life can be pretty and lovely and enjoyable, and I will feel that way again. I am still capable of feeling those feelings, after all. It was a reminder I didn’t know I needed.
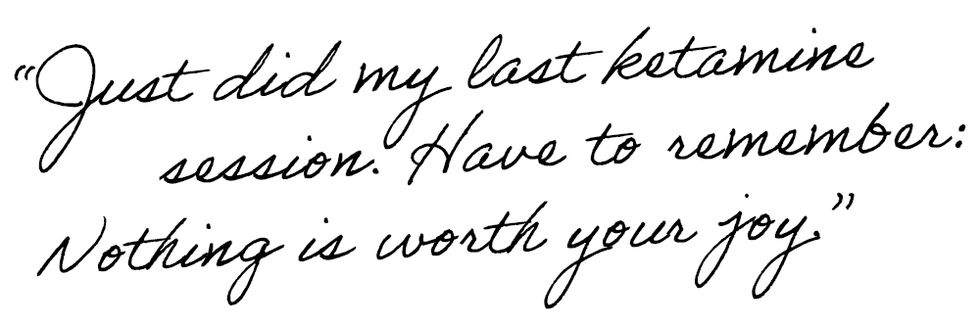
Following the end of my treatment, this is what I scrawled in my journal—a fitting reminder for the start of a new year, and a new chapter.
Meg is the Associate Fashion Commerce Editor at ELLE.com where she researches trends, tests products, and looks for answers to all your burning questions. She also co-writes a monthly column, Same Same But Different. Meg has previously written for Cosmopolitan and Town & Country. Her passions include travel, buffalo sauce, and sustainability. She will never stop hoping for a One Direction reunion tour.


Your articles are very helpful to me. May I request more information? http://www.ifashionstyles.com